- Home›
- Pharmaceuticals›
- Injections›
- Powder for Injection›
- Vancomycin for Injection
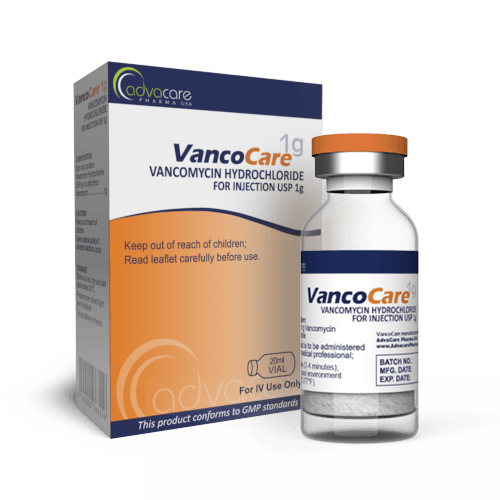
Vancomycin for Injection
Dosage
Packaging
What is Vancomycin?
Active Ingredients: Vancomycin HCl
Vancomycin HCl for Injection is an antibiotic drug used to treat severe infections caused by susceptible bacteria. It is indicated for the treatment of severe staphylococcal infections, endocarditis, osteomyelitis, pneumonia, septicemia, skin and skin structure infections, and infections of the intestines.
Vancomycin belongs to a group of medicines called glycopeptide antibiotics. Its primary bactericidal action results from the inhibition of cell wall biosynthesis. Vancomycin binds to sites on two peptides (N-acetylmuramic acid and N-acetylglucosamine) that are essential for forming the major structural component of gram-positive bacterial cell walls. The incorporation of these subunits into the peptidoglycan matrix is prevented, resulting in the inhibition of cell wall synthesis and cell division. Vancomycin has additional bactericidal action from its impacts on cell membrane permeability and RNA synthesis.
AdvaCare Pharma is a manufacturer and supplier of Vancomycin HCl. Every part of our supply chain is thoroughly vetted to ensure it meets health, safety, and environmental standards. This drug is produced in our GMP-certified facilities in China, India, and the USA.
Why choose us as your Vancomycin manufacturer?
AdvaCare Pharma, a US-owned pharmaceutical company, is a manufacturer of Vancomycin for Injection with GMP-compliant manufacturing facilities located worldwide. We conduct frequent GMP, third-party and internal facility inspections to ensure that our manufactured injectable treatments exceed the stringent requirements of importing countries and our distributors.
As a renown Vancomycin manufacturer and global supplier of 120+ pharmaceutical injection products, our global reach extends to over 65 markets ensuring that pharmaceutical distributors, hospitals, pharmacies, NGOs and government institutions receive the quality-assured treatments they need.
Uses
What is Vancomycin used for?
It is used to treat bacterial infections such as:
- severe staphylococcal infections
- endocarditis
- osteomyelitis
- pneumonia
- septicemia
- skin and skin structure infections
- intestinal infections
This medication is sometimes used off-label as surgical infection prophylaxis.
How is Vancomycin for Injection used?
This medication is manufactured as a powder, which is packaged in a vial. As an injectable form, it is to be given intravenously (IV). Reconstituted solutions should be used immediately.
What dose should be given and for how long?
Adults The usual daily IV dose is 2g, given as either: 500mg every 6 hours; or 1g every 12 hours. Infusions should not be administered at rates exceeding 10mg/min or over a time-period less than 60 minutes.
Children (> 1 month; < 50kg) The usual IV dose is 10mg/kg, given every 6 hours. Infusions should not be administered over a time-period less than 60 minutes.
Neonates (≤ 1 month) The recommended initial dose is 15mg/kg. For neonates in the first week of life, further infusions should be 10mg/kg, given every 12 hours. After the first week and up to the age of 1 month, further infusions can be given every 8 hours. Premature neonates may require dosage reductions, as vancomycin clearance decreases as postconceptional age decreases. Infusions should not be administered over a time-period less than 60 minutes.
For surgical prophylaxis in all patients, the usual dose is 15mg/kg, given over 1-2 hours. Treatment should begin 2 hours before surgery.
The exact dosage is based on the severity of the infections, age, sex, and weight. Refer to a doctor or pharmacist for guidelines on dosage.
Who can use Vancomycin?
Vancomycin can be administered to patients of any age, but caution is advised for specific groups of patients.
Pregnant One study of vancomycin use in a limited number of pregnant patients did not note neonate ototoxic or nephrotoxic effects, even though vancomycin was found present in cord blood. It is unknown whether vancomycin has the potential to cause fetal harm, as it was only administered in the second and third trimester. Vancomycin should only be used during pregnancy if deemed medically necessary.
Nursing Vancomycin is excreted in human milk in small amounts. The potential effects on nursing infants are unknown. It is poorly absorbed orally and is unlikely to reach the bloodstream and cause adverse effects. Vancomycin is likely safe to use while nursing.
Pediatric In pediatric patients, concomitant administration of vancomycin and anesthetic agents has been associated with erythema and histamine-like flushing. Close monitoring of vancomycin serum concentrations may be necessary in pediatric patients (> 1 month) and is recommended in neonates.
Geriatric Due to age-related decreases in renal function, dosage reductions may be necessary when treating older patients.
Other warnings
Vancomycin may increase the risk of acute kidney injury (AKI). In patients with renal insufficiency, dosage reductions may be necessary. Renal function should be monitored in all patients receiving vancomycin, especially those with present renal impairment, comorbidities associated with renal impairment, and those receiving concomitant therapy with other nephrotoxic medications, such as amphotericin B, aminoglycosides, bacitracin, cisplatin, colistin, polymyxin B, or viomycin.
Vancomycin should be infused over a time-period of no less than 60 minutes to avoid rapid-infusion reactions, such as hypotension, erythema, urticaria, pruritus, flushing, and shock. Concomitant administration with anesthetic agents can increase the frequency of these events and may cause anaphylactoid reactions in patients with hypersensitivities. Vancomycin should be administered prior to anesthetic induction to potentially minimize or prevent these events.
Ototoxicity that may be temporary or permanent has occurred in patients receiving vancomycin. These effects have mostly occurred in patients who were given excessive doses, had underlying hearing loss, or were concomitantly receiving other medications with ototoxic effects, such as an aminoglycoside.
In hypersensitive patients, there is a potential for serious dermatologic reactions, such as toxic epidermal necrolysis (TEN), acute generalized exanthematous pustulosis (AGEP), Stevens-Johnson Syndrome, and linear IgA bullous dermatosis (LABD). Cases of drug reaction with eosinophilia and systemic symptoms (DRESS) have also been reported. If signs or symptoms of skin rashes, mucosal lesions, or blisters occur, vancomycin should be discontinued immediately.
Clostridium difficile-associated diarrhea (CDAD) has been documented following the administration of various antibiotic agents, including vancomycin, with manifestations ranging from mild diarrhea to severe colitis, and, in extreme cases, fatality. The use of antibiotics can disrupt the normal flora of the colon, paving the way for the overgrowth of C. difficile. Specific strains of C. difficile can significantly elevate the risks of morbidity and mortality. Individuals experiencing diarrhea weeks to months after concluding vancomycin treatment should be closely monitored for CDAD. If CDAD is suspected or confirmed, the continued use of antibiotics not targeted at C. difficile may require cessation. Adequate management involving fluid and electrolyte balance, protein supplementation, antibiotic therapy targeting C. difficile, and, when clinically warranted, surgical assessment should be promptly initiated.
Reversible neutropenia has been reported in patients receiving vancomycin. Leukocyte counts should be monitored in patients receiving prolonged vancomycin treatment or those concomitantly receiving medications that may cause neutropenia.
Vancomycin is irritating to tissue and must be administered by a secure IV route. Pain, tenderness, and necrosis occur if vancomycin is unintentionally injected into surrounding tissue or leaks from a vein. Thrombophlebitis may occur at injection sites; its frequency and severity can be minimized with slow drug infusion and rotation of venous access sites.
Hemorrhagic occlusive retinal vasculitis (HORV), which may result in permanent loss of vision, has occurred in patients receiving intracameral or intravitreal administration of vancomycin during or after cataract surgery. The safety and efficacy of administering vancomycin via these routes have not been established by adequate and well-controlled trials. Vancomycin is not indicated for prophylaxis of endophthalmitis.
The safety and efficacy of vancomycin administration via intrathecal (intralumbar or intraventricular) or intraperitoneal routes have not been established by adequate and well-controlled trials.
Vancomycin administered via the intraperitoneal route during continuous ambulatory peritoneal dialysis (CAPD) has reportedly resulted in a syndrome of chemical peritonitis. This syndrome can result in cloudy dialysate, which can be present with or without varying degrees of abdominal pain and fever, and appears to resolve after intraperitoneal vancomycin discontinuation.
Administering vancomycin in the absence of a proven or strongly suspected bacterial infection or prophylactic indication is unlikely to provide any clinical benefit and increases the risk of developing drug-resistant bacterial infections.
Side Effects
As with all pharmaceuticals, some unwanted effects can occur from the use of Vancomycin HCl for Injection.
Common side effects include, but may not be limited to: • pain or other reactions at injection site
Serious side effects may occur. Seek medical attention if the following develop:
- signs of an allergic reaction (rash, hives, itching)
- muscle spasms or twitching
- red-neck or flushing (related to the infusion rate)
For a comprehensive understanding of all potential side effects, consult a medical professional.
If any symptoms persist or worsen, or you notice any other symptoms, please call your doctor.
Precautions
Do NOT use Vancomycin HCl for Injection if: • You are allergic to any of the ingredients.
Before treatment, consult your doctor regarding any medications you are taking to address potential drug interactions.
This medication may not be suitable for people with certain conditions, regularly monitoring the kidney function and dosage adjustments may be necessary based on the patient's renal function, so it is important to consult with a doctor if you have any health conditions such as kidney failure.
Rapid administration by bolus may be associated with exaggerated hypotension. It is best to administer this injection using a slow rate.
Vancomycin 500mg: Why the most common dose?
Vancomycin 500mg is prescribed for its efficacy in treating bacterial infections, including those caused by MRSA and other resistant strains. This dosage provides effectual treatment while allowing for careful monitoring of patient response. For more severe infections, Vancomycin 1g is often used.
References
Local Application of Vancomycin in One-Stage Revision of Prosthetic Joint Infection Caused by Methicillin-Resistant Staphylococcus aureus
The main objective of this study is to evaluate the effectiveness and safety of intraarticular (IA) injection of vancomycin in the control of MRSA PJI after one-stage revision surgery in a rat model.
Two weeks of intraperitoneal (IP) and intraarticular injection of vancomycin can control the infection after this surgery. The vancomycin injection can lead to better outcomes in skin temperature, bacterial counts, biofilm on the prosthesis, serum α1-acid glycoprotein levels, residual bone volume, and inflammatory reaction in the joint tissue, compared with those treated with IP vancomycin.
The conclusion of this study is that intra-articular (IA) administration of vancomycin is both effective and safe, proving to be superior to systemic administration. Both IA and systemic vancomycin treatments can eradicate the infection with a 2-week treatment regimen.
You might be interested in...
Why AdvaCare Pharma?
As an industry leader, we are aware of our responsibility to provide affordable and sustainable solutions to improve healthcare worldwide.